 Pregnancy meal planners: trimester by trimester - BabyCentre UK
Pregnancy meal planners: trimester by trimester - BabyCentre UK
A healthy diet is very important during pregnancy. good nutrition plays an important role in the health of mothers and babies. As a mother-to-be, you have a higher nutritional needs than you do before conception. However, the general principles of good nutrition-variety, balance and moderation still prevails during pregnancy.
This resource will help you learn how to eat healthy during pregnancy. This includes how to choose a variety of healthy foods, maintaining a healthy weight during pregnancy, and live food-safe.
Eat a balanced diet before, during, and after pregnancy is one part of good health. This section covers the key nutrients pregnant women need and where to find them.
Calories (aka energy for the body) requiring increased during pregnancy. But "eating for two" only requires an additional 340 calories during the second trimester and 500 calories in the third trimester. The first trimester does not need the extra calories.
Choose foods and beverages are "nutrient dense". This means that they are a good source of building blocks your body needs. nutrient dense foods are full of vitamins, minerals and other nutrients. Eat a variety of foods from the five food groups. These include whole grains, vegetables, fruits, milk, and meat and beans. This will ensure that you and your growing baby get the nutrients you both need.
nutritional and caloric needs are higher if you are carrying more than one baby. Discuss what and how much to eat with your health care provider.
Protein helps keep the muscles and tissues of the body. It is also important for the baby's growth - especially during the second and third trimesters. Most pregnant women should take in about 70 grams of protein every day to meet their minimum needs. Keep in mind you may need more than that. protein needs vary by weight and activity level. Talk with your doctor if you have any questions about your daily protein intake. lean meats, poultry, fish, eggs, dairy products, and legumes (beans) is a good source of protein. These foods also provide iron, B vitamins and other essential nutrients. dried beans, nuts, legumes, and soy products like tofu are other sources of protein.
If you're a vegetarian, you can meet your protein needs by eating food that is a complete protein source. A complete protein contains all the essential "building blocks" (amino acids) your body needs. Every day, eat a variety of protein sources to provide your body with essential amino acids. Selection of vegetarian protein include nuts, milk, yogurt, eggs, and soy products. Greek yogurt is a good choice. It has twice the amount of protein when compared with regular yogurt. pregnant vegan can meet their protein from soy, a source of complete protein. Sources of soy protein include soy milk, soy cheese, soy yogurt, tofu, and tempeh. Vegan food samples other protein-rich beans and beans (kidney beans, chickpeas, black beans, etc.).
Carbohydrates are the main source of energy for the body. Fruits, vegetables, grains, and dairy products contain carbohydrates. grains are an important source of nutrients, such as dietary fiber. They also provide a variety of health benefits. Other important carbohydrate foods including fortified refined grains. This item has the added benefits of iron and folic acid, two important nutrients for the developing baby. Many carbohydrate foods are a good choice for breakfast. Including English muffins, yogurt, bagels, cereals, breads, and fruits. choice other carbohydrate-containing meals or snacks including crackers, breads, and pasta.
Aim to get most of your daily calories from carbohydrates. For most people, carbohydrates should make up about 45 to 65 percent of daily caloric intake. Most pregnant and lactating women need about 175-210 grams of carbohydrates per day.
The fat is the key to good nutrition, health, and storage of many important vitamins. Such as carbohydrates and protein, dietary fat is an important energy source for the body. certain foods containing fats supply the body with essential fatty acids. Essential fatty acids are fats that the body does not make, so they should be included in the diet. Most important, essential fatty acids are essential to the growth and development of infants.
Health experts recommend keeping total fat intake between 20 and 35 percent of total calories. Most fat should come from unsaturated sources. Sources of unsaturated fats include fish, vegetable oils (canola, soybean, olive, peanut, safflower, and sunflower oil), nuts, and flaxseed. All women, including those who are pregnant or nursing should follow these recommendations.
DHA are unsaturated fats that are important for infant brain and eye development. Pregnant women should aim to get 200 mg of DHA per day. Oily fish such as salmon and tuna contains DHA. For example, a serving of salmon (3.5 ozor roughly the size of a deck of cards) have more than 1 gram of DHA. This is five times the recommended amount. A health care provider may recommend a dietary supplement or prenatal vitamin with DHA. For more information about eating fish during pregnancy, see section Food Safety.
Calcium is important for bone growth and teeth strong. Calcium intake is necessary for all women. especially pregnant women younger than 25 years old whose bones are still growing.
Pregnant women should aim to consume 1,000 mg of calcium per day. It is about three servings of calcium-rich foods. Female 18 years need 1,300 mg per day, or four servings of high-calcium foods. Many women do not get enough calcium, so it is important to focus on foods rich in calcium. Women who do not consume dairy products should consider a calcium supplement or a multivitamin.
Dairy products like milk, yogurt and cheese are good sources of calcium. Non-fat (skim) and low-fat (1%) milk has the same amount of calcium and fewer calories than higher-fat (2% and whole) milk.
Other sources of calcium include dark green, leafy vegetables, dried beans and peas, nuts and seeds, and sardines. food and beverages fortified with calcium are also a good source of calcium. This includes some orange juice, soy milk, tofu, almond milk, and breakfast cereals. It is easiest to meet your calcium needs through dairy products. If you are vegetarian, have lactose intolerance or milk allergies, ask your health care provider how to consume adequate calcium.
Pregnant women should not consume raw (unpasteurized) milk or eat foods containing raw milk. Raw milk may increase the risk of foodborne disease is very dangerous, including listeriosis. For more information, see the section of this source of Food Safety.
Vitamin D is important for calcium absorption, immune function and brain health. Sunlight is one source of vitamin D. About five to ten minutes of sunlight on exposed arms or face can provide a day's worth of Vitamin D. This time may vary depending on geographic location and the color of your skin. Aiming to fifty mcg, or 2,000 IU of vitamin D per day. This objective can be met with a multivitamin. Milk or yogurt with added vitamin D can help you meet your daily needs. fish oil, mushrooms, cereals, and dietary supplements also contain vitamin D.
Iron carries oxygen through the blood and give the whole body. It also helps in immunity, brain development, and metabolism. About 90 percent of the iron in the body is recycled every day. The growing baby also save enough iron to last through the first few months of life.
The pregnant woman has an increased amount of blood in their body so they need more iron than women who are not pregnant. Pregnant women should aim for a total of 45 mg of iron per day from food and dietary supplements. animal products, including red meat, fish, poultry, and eggs, which are rich in iron. Other options include fortified breads and whole grains, cereals, and pasta. green leafy vegetables, beans, nuts, eggs, and dried fruits are also a good source.
Type iron found in animal products different from iron found in plant sources. the body does not absorb iron in plant sources as well as the iron in meat, fish, and poultry. But it can increase the iron absorption when eaten with foods high in vitamin C (such as orange juice or red peppers). A registered dietitian can recommend iron-rich foods and foods that can help the absorption of iron.
Many women enter pregnancy with low iron reserves. Your doctor may recommend iron supplements beginning at the first prenatal visit. Some women also may need screening for iron deficiency in a sustainable manner. Take iron supplements between meals, with water or juice, and not with other supplements. Substances in coffee, tea, and milk can inhibit the absorption of iron. Taking iron supplements at bedtime may help reduce abdominal pain and / orheartburn.
Folic acid, a B vitamin that is needed to help the baby grow, is a key before and during pregnancy. Folic acid reduces the risk of spina bifida and other birth defects of the brain and spinal cord, also called neural tube defects (NTDs). "Folate" is a term for various forms of nutrients found naturally in foods. "Folic acid" is the form used in supplements and products enriched grains.
Enriched bread, flour, pasta, rice, cereals, and other grain products are common food sources of folic acid. To see if your food contains folic acid, check food labels to see whether food containing folic acid or folate.
Each planning pregnant women should consume 400 micrograms (mcg) of folic acid daily to help prevent birth defects. This is along with eating foods that contain folate. Women who had babies with NTDs in the past should take 4 mg per day of folic acid before becoming pregnant again.
There are many ways to meet the folate / folic acid needs you. First, take a multivitamin with folic acid. Also, be sure to eat plenty of fruits and vegetables, products enriched grains, legumes (such as peanuts), citrus fruits and juices.
coffee, tea, energy drinks, some soft drinks, chocolate, and some over-the-counter caffeine. Pregnant or not, it is important to estimate your total caffeine intake from all sources. Caffeine from food and beverage able to cross the placenta and be part of the ASI. However, most of the research findings that pregnant and nursing mothers can safely consume moderate amounts of caffeine. Moderate caffeine intake during pregnancy was about 200 mg / day, which is equivalent to about two cups of 8 ounces of coffee or four cups of tea a day. A 12-ounce caffeinated soft drinks contain about 37 mg of caffeine, while an 8 ounce energy drinks have about 100 mg. It is important to read labels on food and drinks to be aware of how much caffeine they contain.
Some women may have heard about the link between caffeine and miscarriage. There are many studies on whether caffeine increases the risk of miscarriage. But the result is not clear. Leading health experts agree that caffeine is 200 mg per day or less during pregnancy is safe. Talk with your doctor about your caffeine intake if you have a history of heart problems or high blood pressure.
Low-calorie sweeteners are safe for the general population, including pregnant women. FDA and other leading authorities reiterated their safety. Eight low-calorie sweeteners permitted for use in foods and as a table sweetener. They are acesulfame potassium (Ace-K), advantame, aspartame, neotame, saccharin, sucralose, monk fruit extract and stevia leaf extract. Studies show that they are all safe to take during pregnancy.
Anyone with phenylketonuria (PKU) should limit their intake of phenylalanine from all sources. These include aspartame. PKU is a genetic disorder that prevents the breakdown of phenylalanine. Phenylanine present in aspartame and many other foods. Pregnant women who have the gene but not the disorder PKU PKU can digest aspartame is safe.
Sodium is, naturally a very important part of the fluids in the human body. Sodium works with other minerals to maintain water balance in the body. It is also important for coordinating the nervous system and muscles healthy.
Sodium requirements and limits for pregnant women is not different from the general population. 2015 Dietary Guidelines for Americans recommends limiting sodium intake to 2,300 mg or less per day. Excessive sodium intake has been linked to high blood pressure, heart disease, stroke, and other health conditions.
A balanced diet to meet the needs of the most nutrients. However, your doctor may suggest you take a multivitamin daily as well. It can also help if you plan to become pregnant. Taken several months before conception, vitamin over-the-counter prenatal can help resolve any nutritional deficiencies.
More vitamin and / or mineral supplements may be important for certain groups. For example, you may need to supplement your diet if you are a strict vegetarian or follow a strict diet. Additional supplements may also be beneficial if you are carrying twins or triplets. Consider taking calcium supplements (600 milligrams per day) plus vitamin D if you are a vegan, are under 25 or do not consume milk. Also, supplements of vitamin B12 (and possibly vitamin D and zinc) to strict vegan.
Pregnant women should not take vitamin A supplements. Excessive levels of Vitamin A can be toxic to the developing baby. You can meet the needs of your vitamin A healthy diet and prenatal multivitamin.
There is no scientific evidence to support the benefits of herbal and botanical products during pregnancy. In fact, some herbal products may have serious side effects for the mother and baby. For this reason, pregnant and nursing women should avoid herbal and botanical supplements.
Drinking alcohol during pregnancy can cause permanent physical, behavioral, and intellectual disability. Do not consume alcohol during pregnancy. Also, women who are trying to conceive should not drink alcohol. Many women do not know they are pregnant until they are four to six weeks into the pregnancy. Drinking even small amounts during this time can expose their developing baby to alcohol. Women should stop drinking as soon as they know they are pregnant.
It is important to track your weight during pregnancy. This helps to ensure that you and your baby healthy. Women who gain too little weight at risk of having small babies (less than 5 1/2 pounds). But women who gain too much weight are at greater risk of having a baby early or have a large baby. Getting too much weight during pregnancy can also cause other health problems. This may include gestational diabetes, high blood pressure, and varicose veins in the mother.
Pregnant women store fat to prepare for breastfeeding. If you are under the target weight of your pregnancy, your health care provider will carefully track your progress. Also, ask your health care provider or a registered dietitian to help with meal planning. This will help ensure that you get the nutrients and calories you need to get the right weight.
Weight-goal advantage was based on prepregnancy weight, height, age, and regular diet. Every woman and every pregnancy is unique. Your health care provider can help you gain weight at a healthy level during pregnancy.
A weight loss of 25 to 35 pounds is normal for women with a body mass index, or BMI, of 18.5 to 24.9 kg / m2 ( "normal weight"). BMI is one way to determine whether you are at the right weight. This tool can determine how much weight you should gain during pregnancy. Women who are under a healthy weight when they become pregnant (BMI <18.5 kg / m2) should aim to get about 28 to 40 pounds. Women with a BMI of 25 to 29.9 kg / m2 ( "overweight") should get no more than 15 to 25 pounds. Go to http://www.cdc.gov/nccdphp/dnpa/bmi/ to calculate your personal BMI.
Women with a BMI over 30 kg / m2 ( "fat") should get no more than 11 to 20 pounds. If you are in this category, a health care provider or a registered dietitian can help you meet this recommendation in a healthy way. The aim to meet the caloric and nutritional needs, while maintaining regular physical activity. Weight gain during pregnancy is not recommended.
If you are carrying more than one baby, on weight gain increases. Women with a BMI of 18.5 to 24.9 kg / m2 should get 37-54 pounds. Women with a BMI of 25 to 29.9 kg / m2 should get 31-50 pounds. Women with a BMI over 30 kg / m2 should aim to get 25-42 pounds. There are no set guidelines for weight gain for underweight (BMI less than 18.5 kg / m2) women carrying more than one baby. Working closely with your health care provider to ensure proper weight.
The pattern of weight gain during pregnancy is as important to the overall weight. The doctor will keep a high note and started heavy on the first prenatal visit. Regular weigh-in will be recorded at each visit to ensure you gain weight at the right level.
weight maintenance or weight loss slightly normal during the first trimester (or the first 13 weeks) of pregnancy. But most women should expect to get about four to five pounds during the first trimester. weight should come from nutrient-rich foods that are described earlier in this resource. Listen to your body signals and stop eating when you feel full. This will help keep you from overeating because "you are eating for two."
Women with a healthy pre-pregnancy weight should gain about a pound a week during the second and third trimesters. Women who are underweight before conception should get a little more than one pound per week. They were initially overweight should gain at a slower rate (a little over half a pound per week).
food cravings and do not like certain foods are common during pregnancy. There is no evidence that food cravings associated with malnutrition. The cause them remains a mystery. It is acceptable to satisfy your food cravings within reason. Especially when they supply nutrients to the diet.
In rare cases, some pregnant women crave non-food substances. It is a disorder called pica. Consumption of goods non-food can be dangerous for mother and baby. In some cases, pica involves eating large amounts of non-food. This can prevent you from getting enough calories or nutrients to stay healthy. Examples of items of non-food, including clay, starch, ice, coffee grounds or baking soda. If you experience cravings for non-food, talk to your doctor immediately. These symptoms may be a sign of nutritional deficiencies (such as Iron), and may need to be treated with supplements.
Physical activity is another important part of good health. Include 30 minutes or more of moderate physical activity on most, if not all, days of the week. Try activities such as walking or swimming. But to avoid activities that have a high risk of falling or injury. If you already do vigorous activity (such as running), you can continue them during pregnancy. Discuss adjustment activities with your health care provider. Some women could not fit 30 minutes of one at a time into their schedules. Feel free to divide time into three 10-minute intervals throughout the day.
Food safety is important to everyone. There are certain foods that pose additional risks to pregnant women and their unborn babies. In particular, pregnant women should be aware of the increased risk of listeriosis.
Listeriosis is a dangerous infection caused by bacteria that are often found in soil, groundwater, and plants. Cooling, ready-to-eat foods such as meat, poultry, seafood, and dairy products may contain listeria. Also, unpasteurized (raw) milk and products made with raw milk can contain these bacteria. Listeria can be dangerous for pregnant women and their unborn babies. Listeriosis, an infection caused by listeria, can cause a lot of harm to the mother and baby. These include premature birth, miscarriage, fetal death and severe disease of the newborn.
Symptoms of listeriosis can take several days or even weeks to appear and may be mild. You may not know you have listeriosis. This makes practicing proper food safety is even more critical. Listeriosis can have flu-like symptoms at first. These include sudden onset of fever, chills, muscle aches, diarrhea, and / or abdominal pain. Other symptoms can include headache, stiff neck, confusion, loss of balance, or convulsions. A blood test can determine if you have listeriosis, and can be treated with antibiotics. It also can prevent the fetus from getting infections.
Avoid certain foods during pregnancy to prevent listeriosis. These include:
fish contains high-quality protein and other essential nutrients. It is also low in saturated fat, and contain healthy omega-3 fats. These fats contribute to heart health, brain development and proper growth and development of children. 2015 Dietary Guidelines encourage pregnant and nursing women to eat 2-3 meals (8-12 ounces) of seafood each week.
All of the popular types of fish in the US are healthy, low in mercury and safe to eat during pregnancy. These include salmon, tuna (canned), and tilapia. All seafood contains traces (very, very small) amount of mercury. But only four types of fish should be avoided during pregnancy because of their mercury content. Higher fish-mercury tilefish, shark, swordfish, king mackerel.
The food has a major role in maintaining the health of mothers and their babies. Nutritional habits and practice good food safety during pregnancy. This can have lifelong benefits for you and your child. Eating a mixture of grains, fruits, vegetables, low-fat dairy, lean meats, and nuts. All the food groups provides important nutrients to your diet. Also, remember that certain foods may pose a health risk for the mother and the unborn baby. Choose foods based on the principles of balance, variety and moderation. This is the best approach to enjoy a healthy eating plan during pregnancy and for a lifetime.
PAS licensed health professionals, and health care team members appreciated that Includes a supervising physician. Personal Assistant provides a variety of medical and surgical services to a diverse population. They can diagnose and treat illnesses, order and interpret tests, developing the treatment plan, and write prescriptions in all 50 states, the District of Columbia, and all US territories, with the exception of Puerto Rico. PAS also advise on preventive health care and assist in the operation.
AAPA is the only national organization to represent the nation's more than 108 500 physician assistants in all clinical specialties. Established in 1968, the Academy works to improve the quality, cost-effective health care, and professional and personal growth of hedge. For more information about the Academy and the PA profession, visit AAPA's Web site, www.aapa.org.
 Pin on Home
Pin on Home Pregnancy meal planners: trimester by trimester - BabyCentre UK
Pregnancy meal planners: trimester by trimester - BabyCentre UK Pin on Pregnancy
Pin on Pregnancy Pin on 21 day fix
Pin on 21 day fix 50 Pregnancy Meal Ideas - Fit To Be Pregnant
50 Pregnancy Meal Ideas - Fit To Be Pregnant First trimester pregnancy diet plan | Living and LovingLiving and ...
First trimester pregnancy diet plan | Living and LovingLiving and ...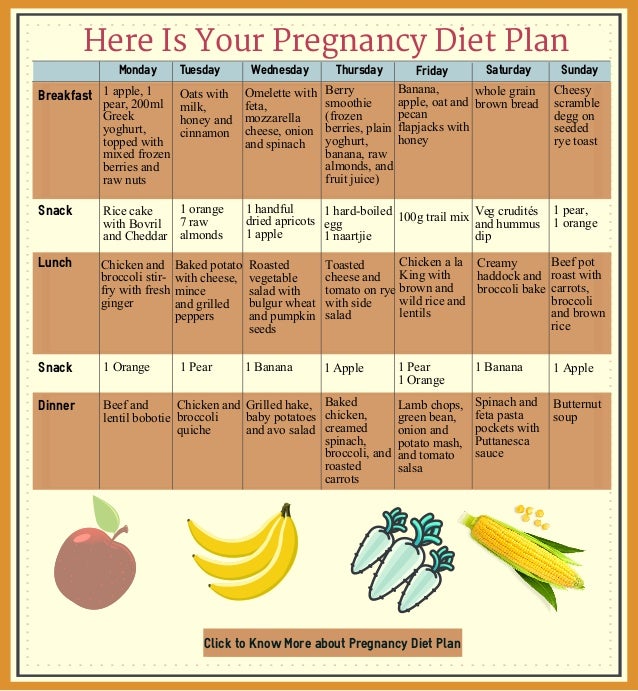 Your Perfect Pregnancy Diet Plan (Pregnancy Meal Plan)
Your Perfect Pregnancy Diet Plan (Pregnancy Meal Plan) Pin on Healthy Pregnancy
Pin on Healthy Pregnancy Pregnancy menu plan: First trimester, vegetarian plan - BabyCenter ...
Pregnancy menu plan: First trimester, vegetarian plan - BabyCenter ... The Pregnancy Seafood Guide: What to Eat for a Healthy Pregnancy ...
The Pregnancy Seafood Guide: What to Eat for a Healthy Pregnancy ... Meal Planning During Pregnancy: What is a Sensible Meal Plan ...
Meal Planning During Pregnancy: What is a Sensible Meal Plan ... SLP Pregnancy Food Plan
SLP Pregnancy Food Plan Your pre-pregnancy diet plan | Living and LovingLiving and Loving
Your pre-pregnancy diet plan | Living and LovingLiving and Loving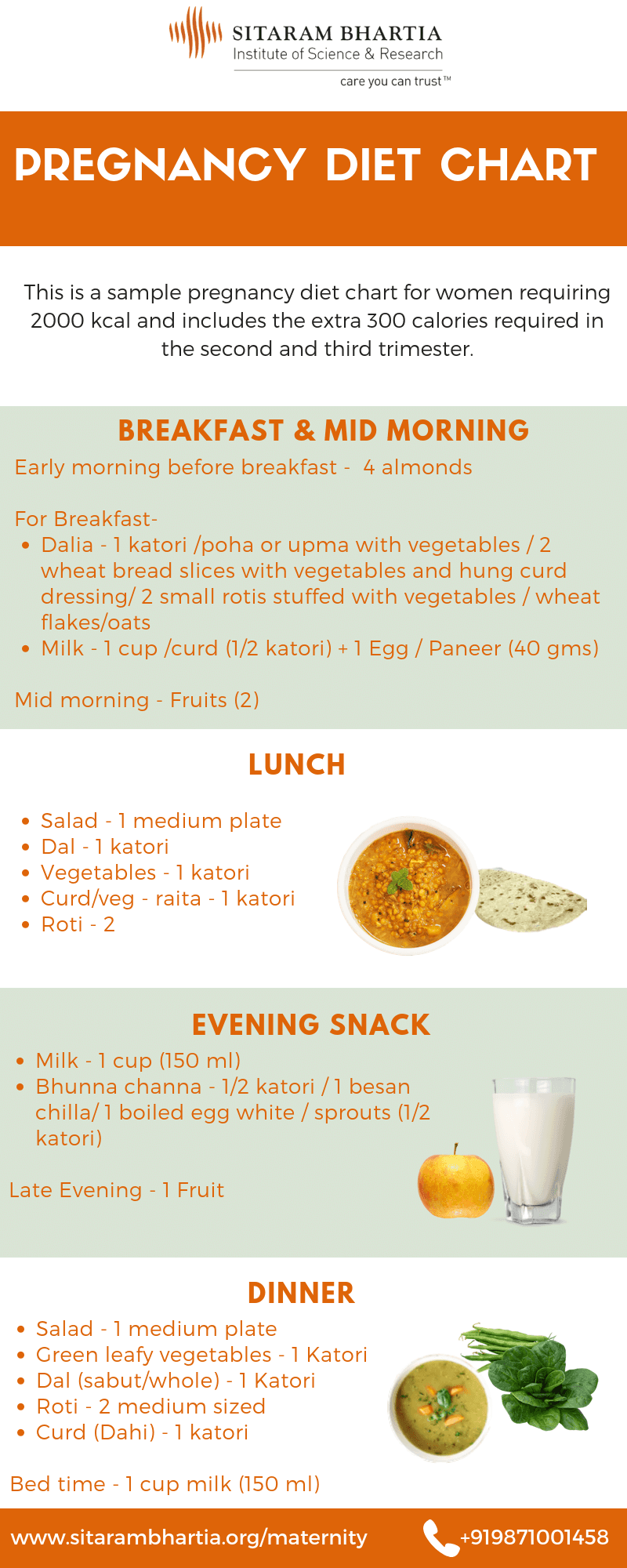 What You Need to Know About Your Pregnancy Diet Chart
What You Need to Know About Your Pregnancy Diet Chart Pregnancy food plan
Pregnancy food plan Pin on Healthy Eating
Pin on Healthy Eating fat loss meal plan women, pregnancy best food, proper daily diet ...
fat loss meal plan women, pregnancy best food, proper daily diet ...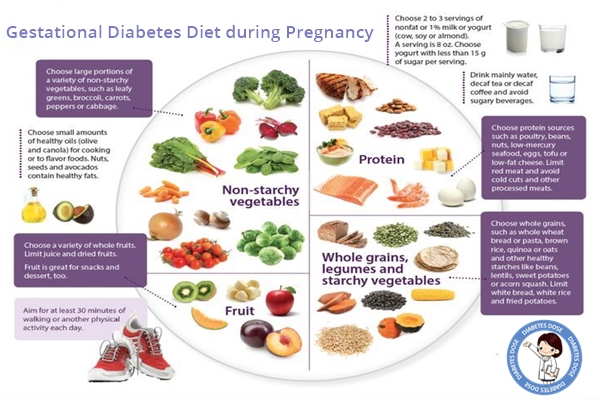 10 Foods to Include in Your Pregnancy Diet if you are suffering ...
10 Foods to Include in Your Pregnancy Diet if you are suffering ... Pregnancy meal planners: trimester by trimester - BabyCenter
Pregnancy meal planners: trimester by trimester - BabyCenter Pregnancy menu plan: Second trimester, plan one - BabyCenter Canada
Pregnancy menu plan: Second trimester, plan one - BabyCenter Canada![Pregnancy diet meal plans for every trimester [Infographic] Pregnancy diet meal plans for every trimester [Infographic]](https://www.smartparents.sg/sites/default/files/image_resources/image-9919752-9860d1b089db8b55a30d80abce7c194b-pregnancy-diet-meal-plan-second-trimester-3.jpg) Pregnancy diet meal plans for every trimester [Infographic]
Pregnancy diet meal plans for every trimester [Infographic] Having a meal plan while pregnant can be very beneficial to both ...
Having a meal plan while pregnant can be very beneficial to both ... Your 7-day pregnancy meal plan | Parent24
Your 7-day pregnancy meal plan | Parent24 Clean Eating Meets Country Girl: Meal planning and being pregnant
Clean Eating Meets Country Girl: Meal planning and being pregnant Nutritionally Fit Meal Plans: Pregnancy | Nutritionally Fit
Nutritionally Fit Meal Plans: Pregnancy | Nutritionally Fit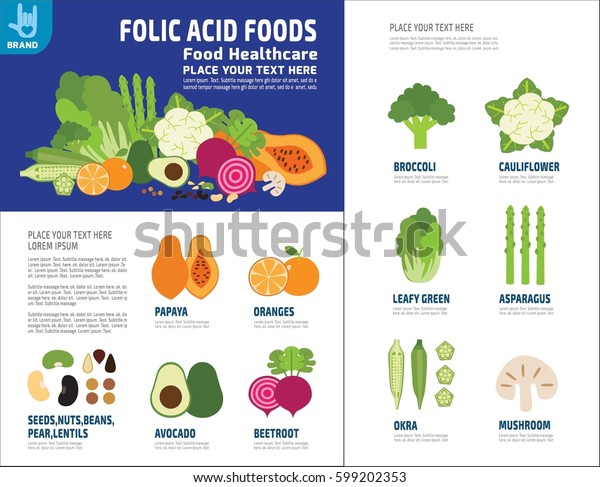 Folic Acid Food Healthy Plan Pregnant | Royalty-Free Stock Image
Folic Acid Food Healthy Plan Pregnant | Royalty-Free Stock Image Pregnancy Diet Ebook
Pregnancy Diet Ebook Pregnancy Meal Planner - Super Seafood
Pregnancy Meal Planner - Super Seafood Hey Mom | Creating a weekly pregnancy menu
Hey Mom | Creating a weekly pregnancy menu![Pregnancy diet meal plans for every trimester [Infographic] Pregnancy diet meal plans for every trimester [Infographic]](https://www.smartparents.sg/sites/default/files/image_resources/image-9919768-39412f7e83282777cb98863a096671a2-pregnancy-diet-meal-plan-first-trimester-2.jpg) Pregnancy diet meal plans for every trimester [Infographic]
Pregnancy diet meal plans for every trimester [Infographic] Diary of a Fit Mommy: Diary of a Fit Mommy's One Week Clean Eating ...
Diary of a Fit Mommy: Diary of a Fit Mommy's One Week Clean Eating ... What Eat While Pregnancy Pregnant Woman Stock Vector (Royalty Free ...
What Eat While Pregnancy Pregnant Woman Stock Vector (Royalty Free ... Pregnancy Meal Plans - EatingWell
Pregnancy Meal Plans - EatingWell How To Create A Healthy Pregnancy Meal Plan - Michelle Marie Fit
How To Create A Healthy Pregnancy Meal Plan - Michelle Marie Fit An Easy Two-Week Meal Plan for the Pregnant Mom | Keeper of the Home
An Easy Two-Week Meal Plan for the Pregnant Mom | Keeper of the Home Pregnancy Meal Plans - EatingWell
Pregnancy Meal Plans - EatingWell The Pregnancy Seafood Guide: What to Eat for a Healthy Pregnancy ...
The Pregnancy Seafood Guide: What to Eat for a Healthy Pregnancy ... Pregnancy Meal Plan For Gestational Diabetes - Pregnancy Diet For ...
Pregnancy Meal Plan For Gestational Diabetes - Pregnancy Diet For ... Diabetic Pregnancy Eating Plan - Diabetic Pregnancy Meal Plan
Diabetic Pregnancy Eating Plan - Diabetic Pregnancy Meal Plan Pregnancy Diet Plan | Healthy Pregnancy Diet Chart - YouTube
Pregnancy Diet Plan | Healthy Pregnancy Diet Chart - YouTube Parentune - Diet Plan/Tips for Third Trimester of Pregnancy ...
Parentune - Diet Plan/Tips for Third Trimester of Pregnancy ... Pregnancy Diet: The Complete Healthy Diet Guide and Nutritious ...
Pregnancy Diet: The Complete Healthy Diet Guide and Nutritious ...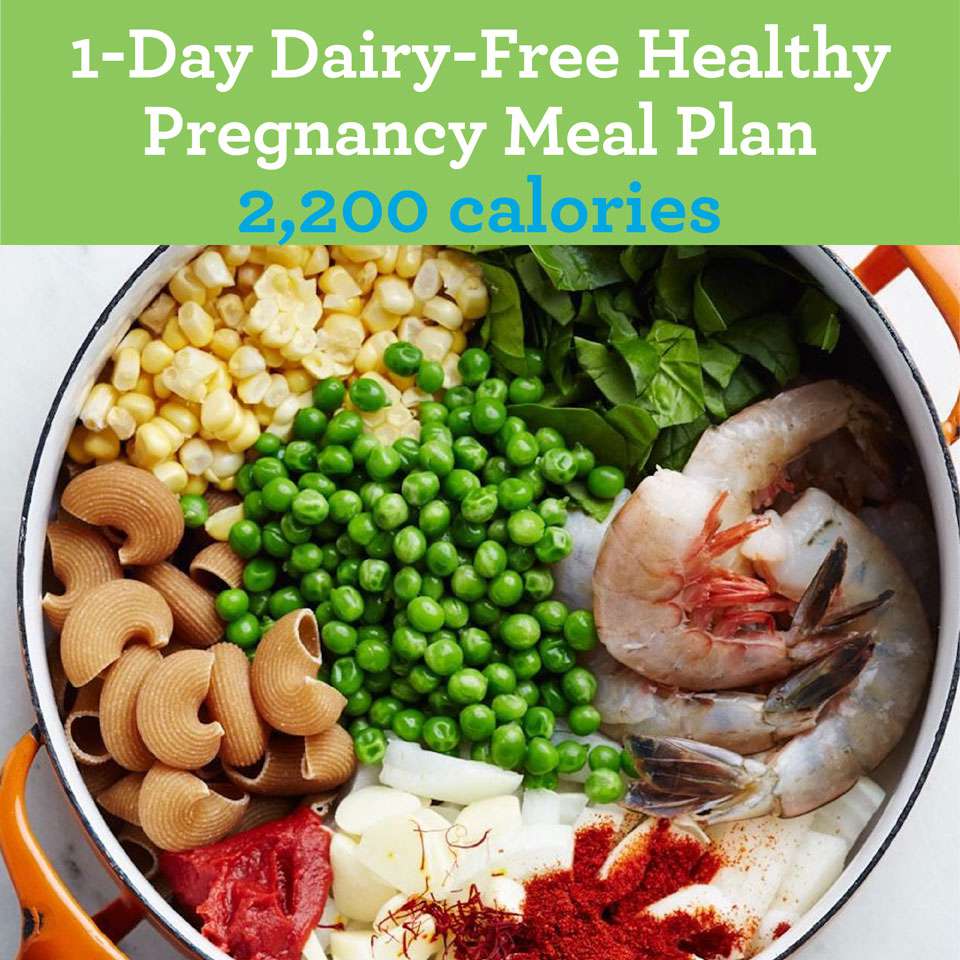 1-Day Dairy-Free Healthy-Pregnancy Meal: 2,200 Calories | EatingWell
1-Day Dairy-Free Healthy-Pregnancy Meal: 2,200 Calories | EatingWell Pin on Food&Drink
Pin on Food&Drink Diet Plan For Gestational Diabetes During Pregnancy - Diet Plan ...
Diet Plan For Gestational Diabetes During Pregnancy - Diet Plan ... The Pregnancy Seafood Guide: What to Eat for a Healthy Pregnancy ...
The Pregnancy Seafood Guide: What to Eat for a Healthy Pregnancy ... Expecting? Here's What You Should Eat (And Avoid) | Westchester ...
Expecting? Here's What You Should Eat (And Avoid) | Westchester ... 1-Day Vegetarian Healthy Pregnancy Meal Plan 2,200 Calories ...
1-Day Vegetarian Healthy Pregnancy Meal Plan 2,200 Calories ... Here's What a Healthy Daily Meal Plan Looks Like
Here's What a Healthy Daily Meal Plan Looks Like Pin on meal plan ideas
Pin on meal plan ideas A Week of Delicious Pregnancy Meals and Snacks | Parents
A Week of Delicious Pregnancy Meals and Snacks | Parents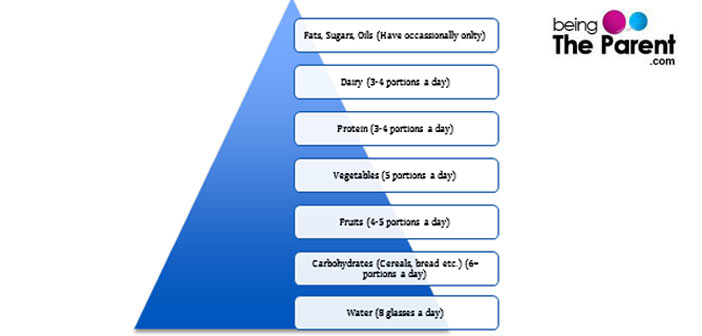 The Pregnancy Food Pyramid - Being The Parent
The Pregnancy Food Pyramid - Being The Parent Diabetes During Pregnancy Diet Plan - Diabetic Pregnancy Meal Plan
Diabetes During Pregnancy Diet Plan - Diabetic Pregnancy Meal Plan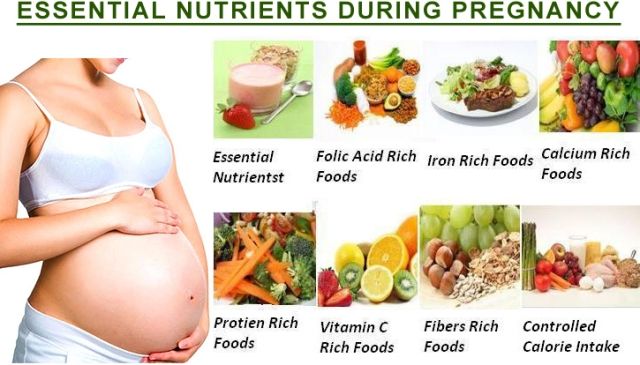 Best Workout Routine & Diet Plan For Pregnant Women | WorkoutInfoGuru
Best Workout Routine & Diet Plan For Pregnant Women | WorkoutInfoGuru The Low GI Eating Plan for an Optimal Pregnancy: The Authoritative ...
The Low GI Eating Plan for an Optimal Pregnancy: The Authoritative ... Pregnancy Meal Plan
Pregnancy Meal Plan 8 Month Pregnancy Meal Planner Template - Microsoft Excel Template ...
8 Month Pregnancy Meal Planner Template - Microsoft Excel Template ... Sample meal plan for pregnancy
Sample meal plan for pregnancy
Posting Komentar
Posting Komentar