 Diagnosing an ectopic pregnancy — The Ectopic Pregnancy Trust
Diagnosing an ectopic pregnancy — The Ectopic Pregnancy Trust
An ectopic pregnancy can be very difficult to diagnose because it often presents with symptoms that can be suggestive of other, more ordinary, conditions such as gastroenteritis, miscarriage or even appendicitis. Doctors rely on women to give them a clear history of their symptoms and the more you can tell your doctor about what had changed, what was different and what is worrying you, the more likely they are to be able to diagnose you. Do not vigilant and take your attention serious symptoms until it actually proved the opposite. If your instincts are screaming at you something that does not feel right, it's OK to trust them and ask medical professionals to reassessment at any time.
EPT assume that all women of childbearing age who experience abdominal pain and / or bleeding should be considered pregnant until proven otherwise.
in diagnosing ectopic pregnancy, medical professionals tend to do some or all of the following tests. Please click on any of your interest and further information will be open.
The first and most basic test is useful for diagnosing ectopic pregnancy is a pregnancy test urine. Because the test is dependent on the hormone Human Chorionic Gonadotropin (hCG), a hormone produced by the fertilized egg after fertilization, this can sometimes result in false-negative results because the hormone is not present in high enough levels to test positive.
whether a woman has a positive urine pregnancy test or not, if he has symptoms of ectopic pregnancy, good practice will then be investigated by ultrasound scan, ideally within 24 hours. sonogram will scan the entire abdomen (belly) first, but it is possible that a transvaginal (internal) ultrasound scans will be required where a special probe is placed into the vagina to get a more detailed look at the reproductive organs.
If during pregnancy scan - which is a pregnancy (gestational) sac, fetal pole and a beating heart - can be seen in the uterus, ectopic pregnancy to live together, while possible, is unlikely. In such cases, the bleeding may be implantation bleeding, bleeding during pregnancy is healthy, or because of impending miscarriage. The pain may be caused by normal, healthy corpus luteum cyst, which forms the ovary after ovulation, the swelling causes pain. Changes in bowel and bladder may be linked to hormonal changes, cause she wanted to urinate (wee) more often and may even be a bit of a constipation (difficult to open the abdomen to have dirt a).
If signs of pregnancy can be seen in the uterus, usually the yolk sac but whether there is an embryo or if the embryo is too small to expect to see a heartbeat, the situation is labeled medical of 'pregnancy Intrauterine from certain Viability' or PUV or IPUV. In this case, you should be offered repeat scan a week to ten days later to check if the baby has developed a heartbeat.
This is a difficult emotional time because it is not clear whether the date for one or whether pregnant women are likely to have a miscarriage. Blood tests will also usually be taken to establish the level of hCG in the blood stream and again 48 hours later, to see how it behaves level.
If no pregnancy can be seen in the uterus, or there is a small gestational sac in the uterus without a yolk sac or embryo, the pregnancy will be medically labeled as pregnancy of Unknown Location or PUL. It is important to understand that the PUL not a diagnosis; it is the label given to the last location of the pregnancy can be identified with certainty. In the event of PUL, blood will be taken to measure serum progesterone and hCG and hCG test was repeated 48 hours later. The doctor will also want to repeat the scan.
Until the definitive location of known pregnancies or serum hormone levels decreased to below the level of pregnancy, there is a risk of complications associated with undiagnosed ectopic pregnancy. For every 100 pregnancies branded as about 10 next PUL be found ectopic; and not all of these needs treatment.
If no pregnancy can be seen in the uterus but no evidence of free fluid in your stomach or maybe 'mass' in the approximate location of your fallopian tubes, the doctor will then tend to diagnose an ectopic pregnancy possible. initial scan will detect more than 70% of ectopic pregnancies.
The hormone Human Chorionic Gonadotropin (better known as hCG) produced during pregnancy by special trophoblast cells, which are found only in the body as a result of implanting a fertilized egg. Increased production of progesterone from the ovaries ovulated prepare the endometrium, but it is that sustains hCG pregnancy.
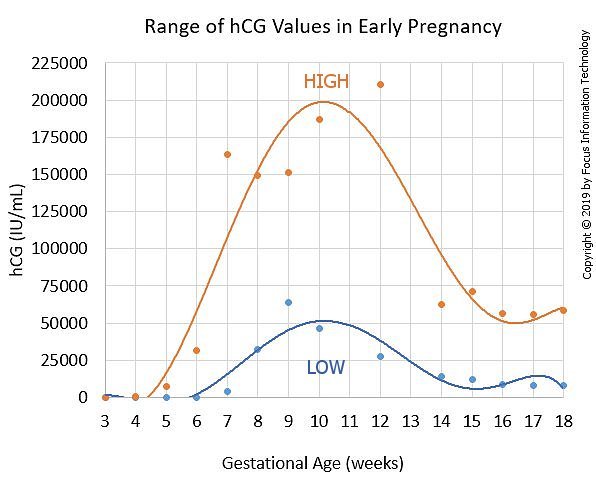
Levels of hCG can first be detected with blood tests normally about 11 days after fertilization, and, in a healthy pregnancy, typically will double every 48 to 72 hours, peaking somewhere between 8 and 11 weeks of gestation (late second early third month) and then plateau or decline and level off for the remainder of the pregnancy it is this increase in initial hCG that sometimes can give the feeling of 'morning sickness' women.
hCG you will only need to be tested if you have reached 6 weeks pregnant and the scan does not clearly show the pregnancy develops in the womb. If the doctor thinks you are a low risk of ectopic pregnancy they can arrange a blood test or urine at intervals or, if they think you are at high risk, they will often repeat test scan or blood within 48 hours and sometimes it can take measurements more before they drawing final conclusions.
The following chart is an example borrowed from the show HSG values for single (one baby than twin) pregnancies. The red line shows the average value of hCG for several days after ovulation (scale at the bottom of the graph). The yellow line shows the bottom of the low range of the value of hCG and the blue line shows the high level of hCG. Green line shows the two HSG test results plotted on a graph, and join them together to show the lines where they sat increase compared to the average.
Doctors at liberty to follow their own protocols hospitals in the UK but there are guidelines in place to help steer medical professionals. For example:
The National Institute for Health and Care Excellence (NICE) was originally established in 1999 to reduce the variation in the availability and quality of NHS care and treatment. In 2005 they joined the Health Development Agency and started to develop public health guidelines. This is a Non-Departmental Public Body sponsored by and responsible to the Ministry of Health even though the guidelines are made by a committee of independent experts.
We are very fortunate to represent the voice of the patient sit on them and consider them to be the first step in improving the diagnosis, treatment and treatment for ectopic pregnancy. They are designed for use by physicians than the general public so that some of the words used may be highly technical.
The Royal College of Obstetricians and Gynecologists (RCOG) encourage the study and advancement of the science and practice of obstetrics and gynecology and the majority of professionals in the field is a member. It produces.
Ectopic Pregnancy Trust gold standard for treatment is that every woman of childbearing age who have symptoms of an ectopic pregnancy should be considered pregnant until proven otherwise. We feel he should receive an ultrasound scan within 24 hours and follow up with the beta hCG blood tests 48 hours apart if the scan is not convincing. Early diagnosis increases treatment options and reduce the emotional trauma associated with the condition and we felt this should always be considered.
If we had been able to help you, if you can help us with a small donation or by volunteering or fundraising?
Ectopic Pregnancy Trust 483 Green Lane London N13 4BS For correspondence course. If you need to send a parcel / package, please contact us for an alternate address
Telephone Helpline :.
Administration & Press:
Reg. Charity: 1071811
We are investigating the emotional impact of ectopic pregnancy. We are also interested in supporting you'll find help from health services or independent sector. Knowledge gained from this study will help support other women and service forms.
Etopic Trust is an ectopic pregnancy regular e-newsletter, with insight into the work we do, charities and how we provide support, raise awareness and support research in an ectopic pregnancy.
We could not have achieved so much without us, who generouslygive their time and skills and provide us with much needed funds through an annual subscription. Most of us are less than £ 10, which only goes to show that even a small amount of ordinary make a very big difference.
Join us at
© 2020 Ectopic Pregnancy Trust ·
 HCG Doubling Time Calculator
HCG Doubling Time Calculator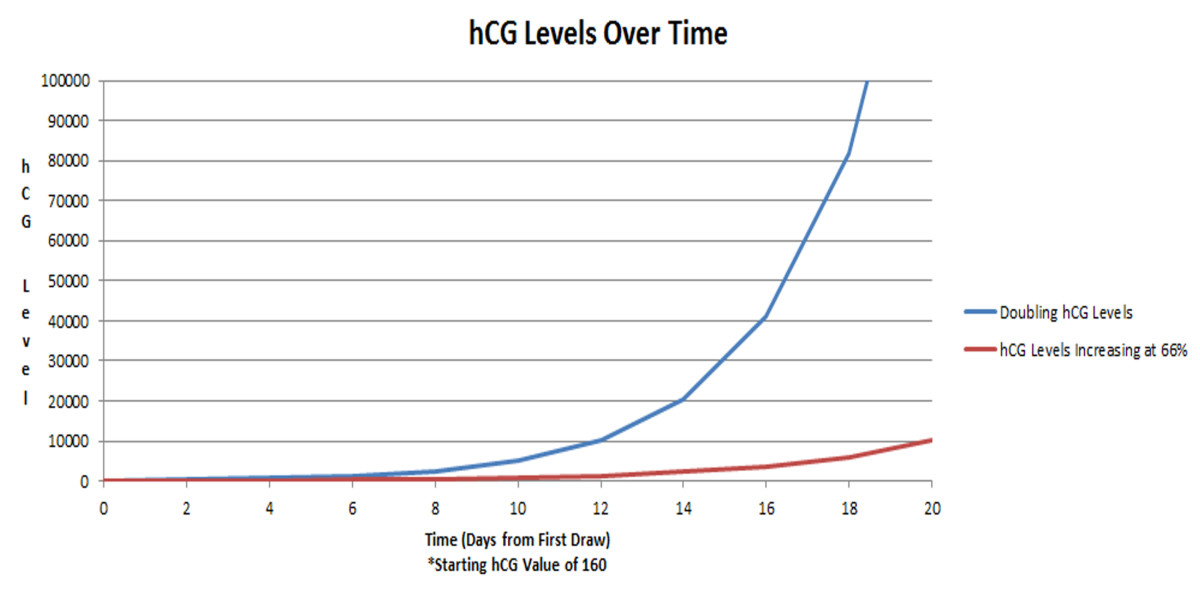 Understanding Tubal Pregnancy and Ectopic hCG Levels | WeHaveKids
Understanding Tubal Pregnancy and Ectopic hCG Levels | WeHaveKids Diagnosis and Management of Ectopic Pregnancy - American Family ...
Diagnosis and Management of Ectopic Pregnancy - American Family ... Flow chart shows methotrexate for ectopic pregnancy workflow ...
Flow chart shows methotrexate for ectopic pregnancy workflow ... Diagnosis and Management of Ectopic Pregnancy - American Family ...
Diagnosis and Management of Ectopic Pregnancy - American Family ... Ectopic Pregnancy - American Family Physician
Ectopic Pregnancy - American Family Physician Pin on Pregnancy
Pin on Pregnancy Early Pregnancy and Painless Spotting - Clinical Advisor
Early Pregnancy and Painless Spotting - Clinical Advisor Diagnosis and Management of Ectopic Pregnancy - American Family ...
Diagnosis and Management of Ectopic Pregnancy - American Family ... Pin on About Early Pregnancy
Pin on About Early Pregnancy Tubal pregnancy - Cancer Therapy Advisor
Tubal pregnancy - Cancer Therapy Advisor Ectopic Pregnancy - American Family Physician
Ectopic Pregnancy - American Family Physician Flow chart shows methotrexate for ectopic pregnancy workflow ...
Flow chart shows methotrexate for ectopic pregnancy workflow ...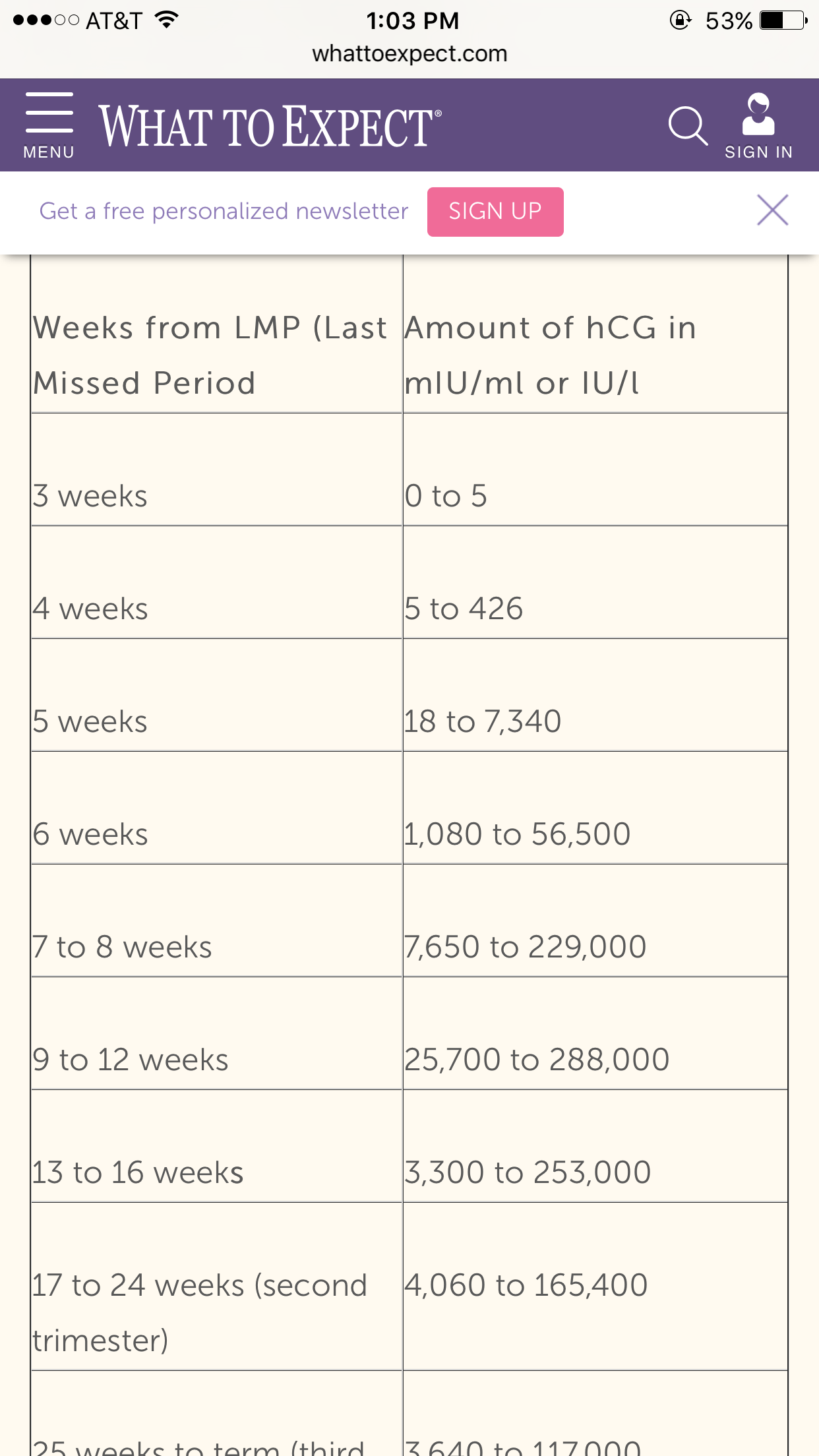 hcg levels chart - Katan.vtngcf.org
hcg levels chart - Katan.vtngcf.org Pin on soups
Pin on soups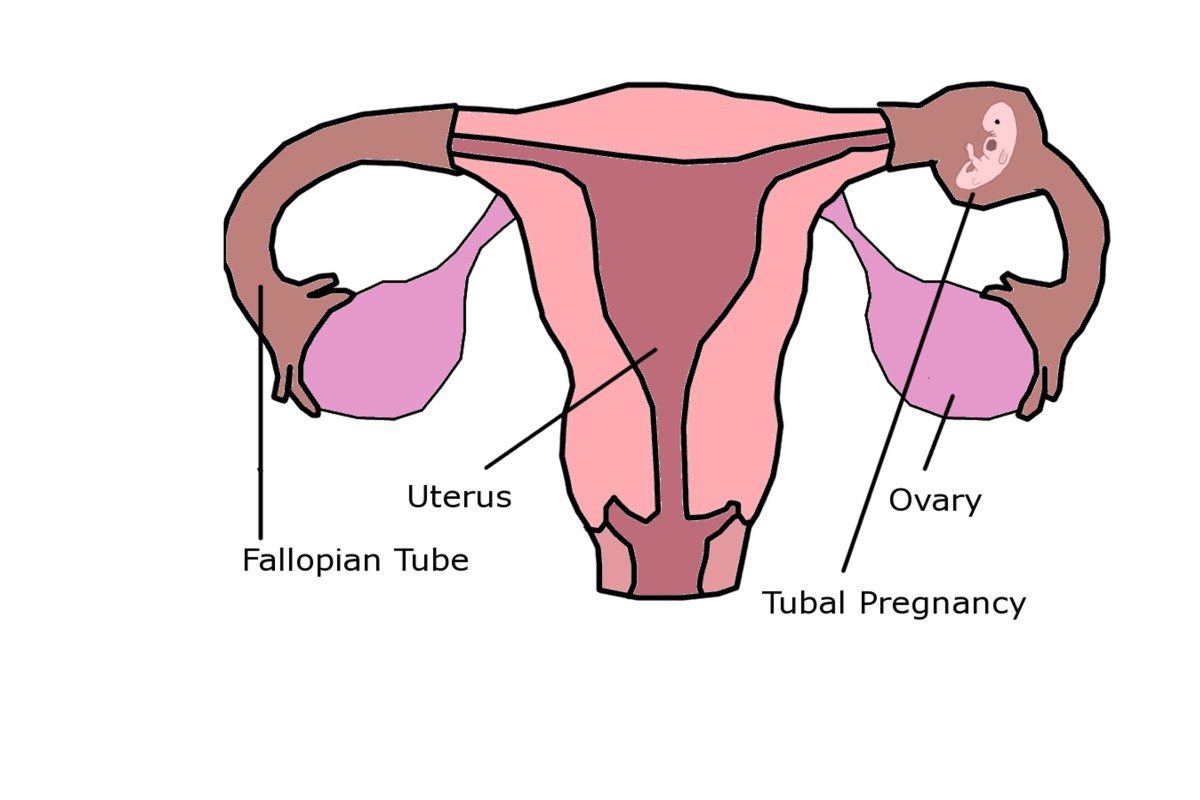 Understanding Tubal Pregnancy and Ectopic hCG Levels | WeHaveKids
Understanding Tubal Pregnancy and Ectopic hCG Levels | WeHaveKids 4 weeks 5 days. HCG Levels and US results have us Worried ...
4 weeks 5 days. HCG Levels and US results have us Worried ... JRM Feature Article
JRM Feature Article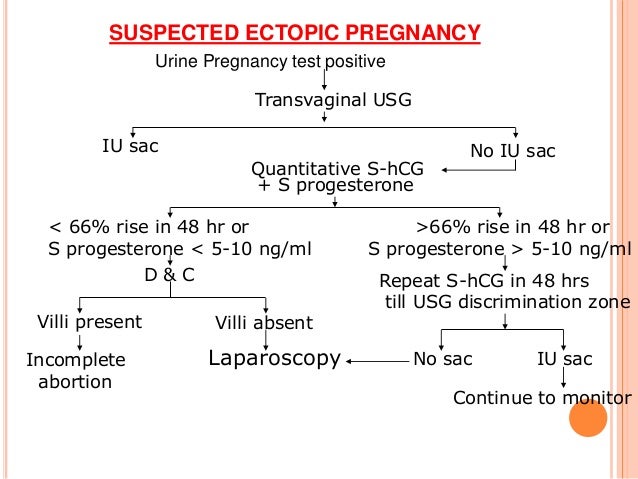 Ectopic pregnancy
Ectopic pregnancy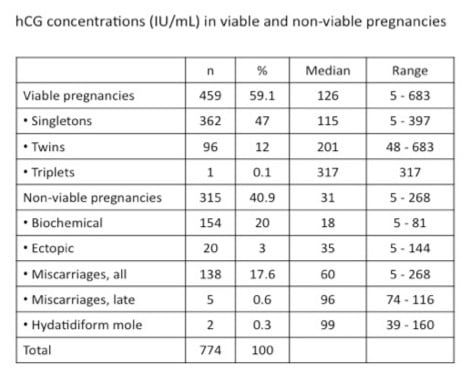 What Does My hCG Level Mean?
What Does My hCG Level Mean?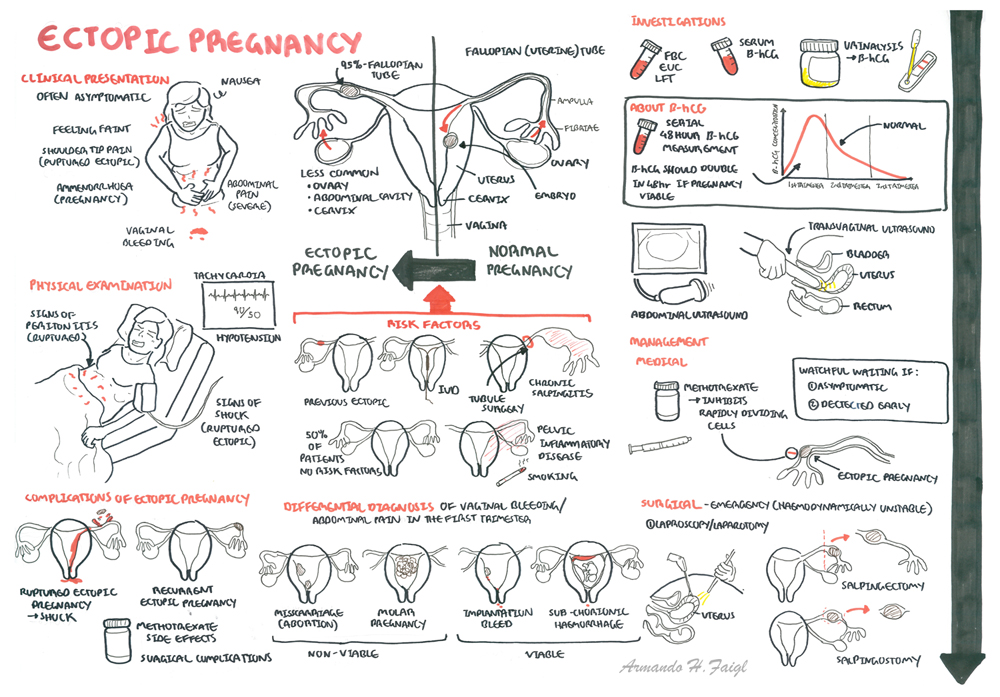 Ectopic Pregnancy | Armando Hasudungan
Ectopic Pregnancy | Armando Hasudungan Diagnosis and Management of Ectopic Pregnancy - American Family ...
Diagnosis and Management of Ectopic Pregnancy - American Family ... Graph with the progression of β-hCG values in the treatment of the ...
Graph with the progression of β-hCG values in the treatment of the ... JRM Feature Article
JRM Feature Article beta results pregnancy chart - Funa.digitalfuturesconsortium.org
beta results pregnancy chart - Funa.digitalfuturesconsortium.org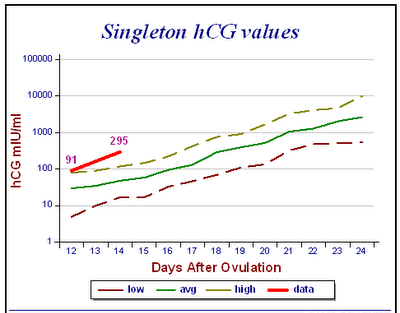 What are Normal Beta hCG Levels? | My Pregnant Health
What are Normal Beta hCG Levels? | My Pregnant Health HCG levels during pregnancy, Ectopic Pregnancy and in Miscarriage ...
HCG levels during pregnancy, Ectopic Pregnancy and in Miscarriage ...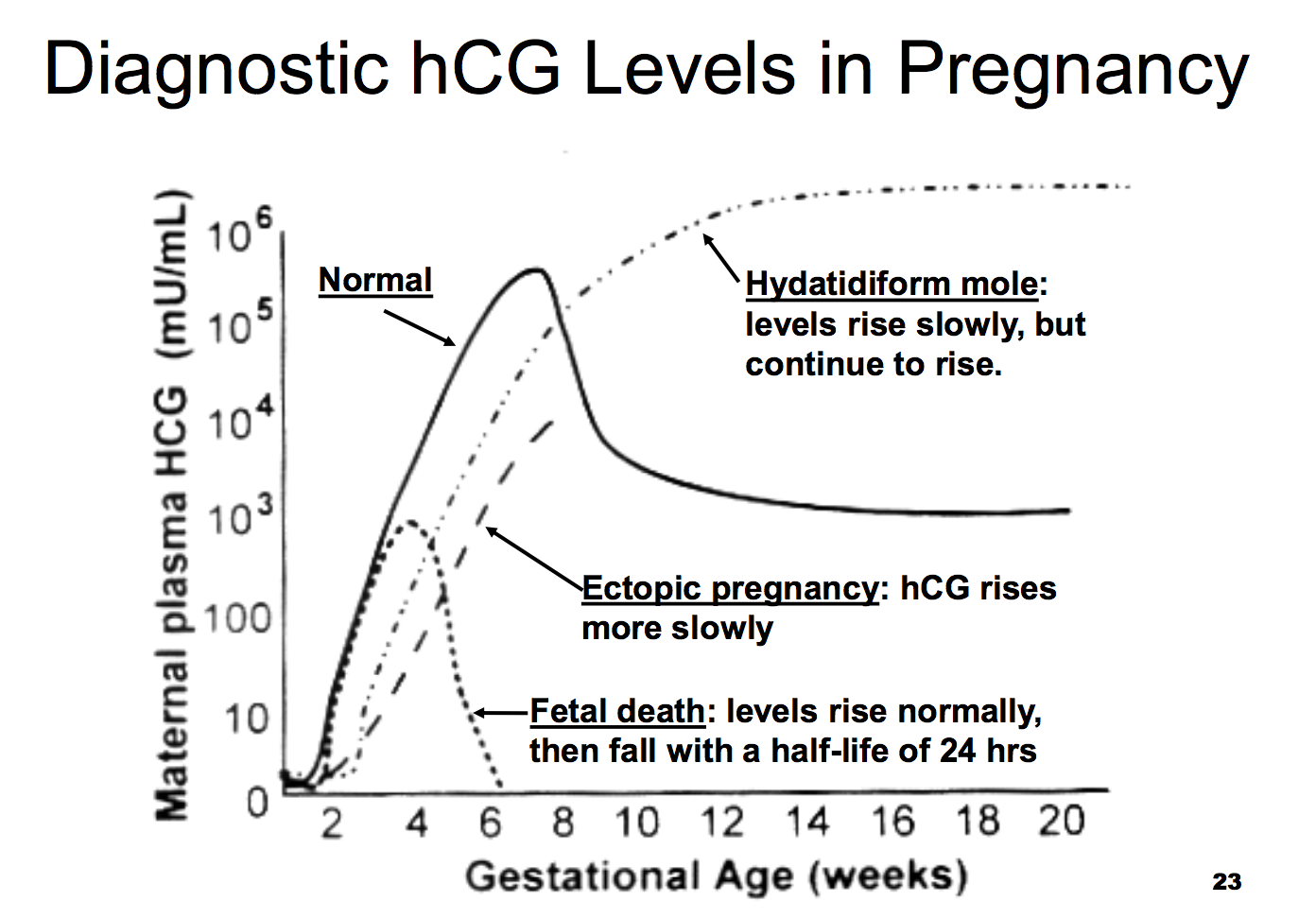 Physiology L46 Fert, Preg, Parturition, and Lactation ...
Physiology L46 Fert, Preg, Parturition, and Lactation ...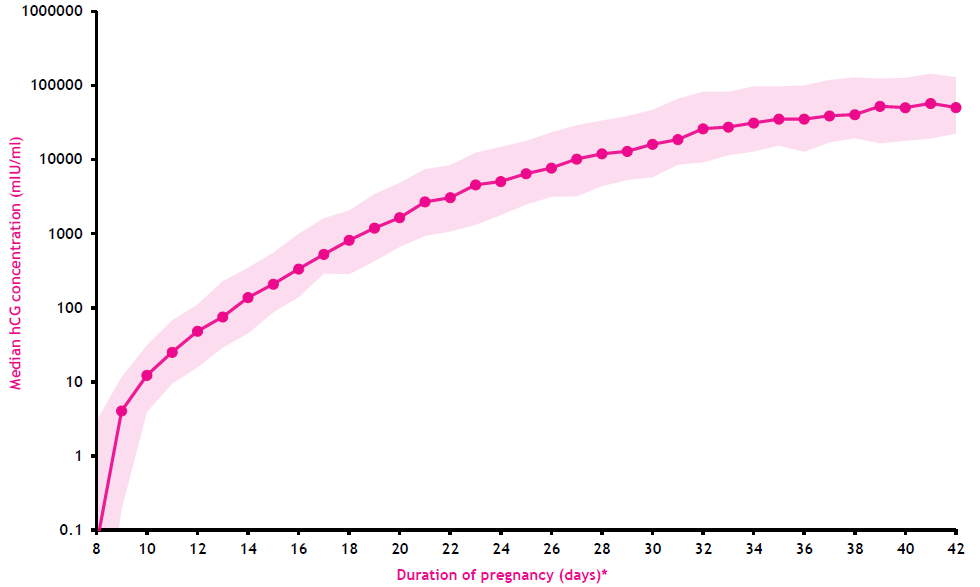 HCG Levels Chart during Pregnancy: Week by Week - Being The Parent
HCG Levels Chart during Pregnancy: Week by Week - Being The Parent Tubal Ectopic Pregnancy - ACOG
Tubal Ectopic Pregnancy - ACOG Do High Beta hCG Levels Mean You're Having Twins | Hcg levels, Hcg ...
Do High Beta hCG Levels Mean You're Having Twins | Hcg levels, Hcg ...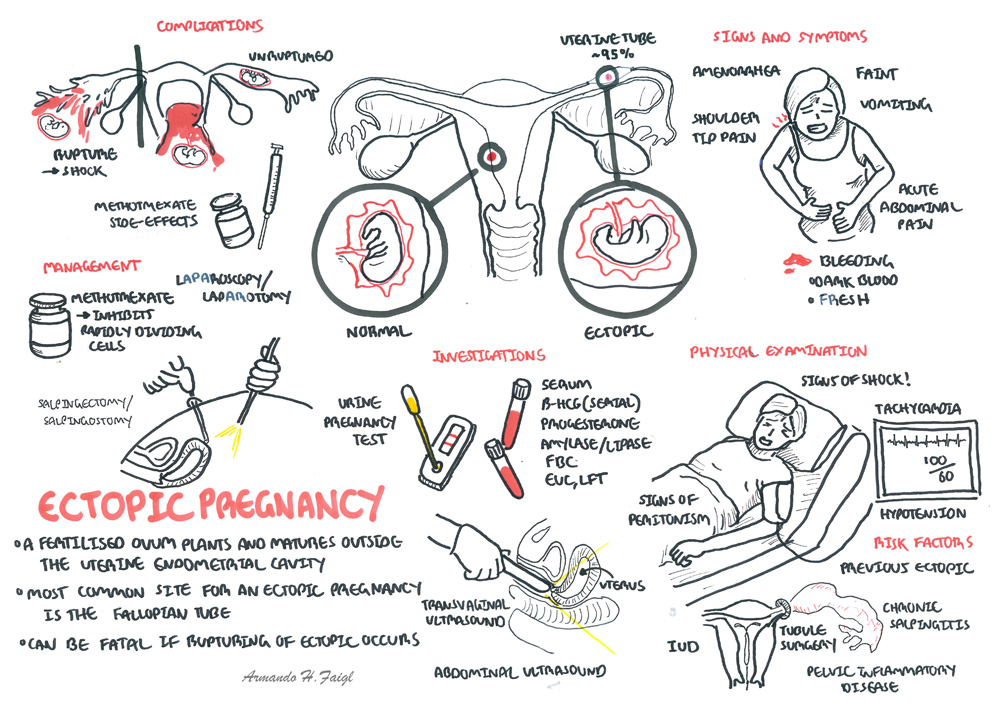 Ectopic Pregnancy | Armando Hasudungan
Ectopic Pregnancy | Armando Hasudungan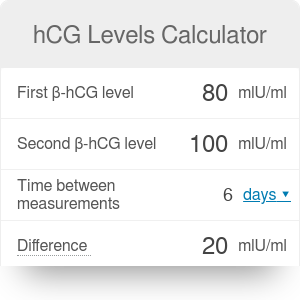 hCG Levels Calculator | hCG Doubling | Chart - Omni
hCG Levels Calculator | hCG Doubling | Chart - Omni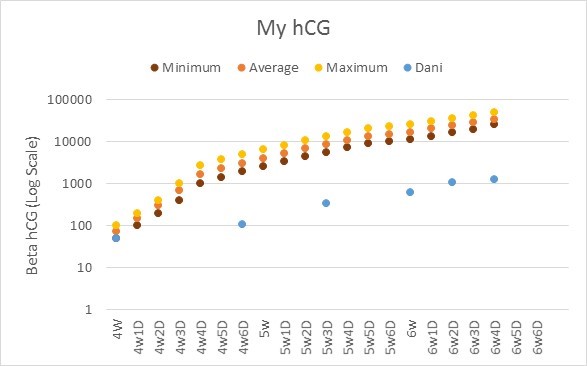 I said NO…am I crazy? – The Great Pudding Club Hunt
I said NO…am I crazy? – The Great Pudding Club Hunt An early beta hCG test does predict your risk of miscarriage ...
An early beta hCG test does predict your risk of miscarriage ... Ectopic Pregnancy | GLOWM
Ectopic Pregnancy | GLOWM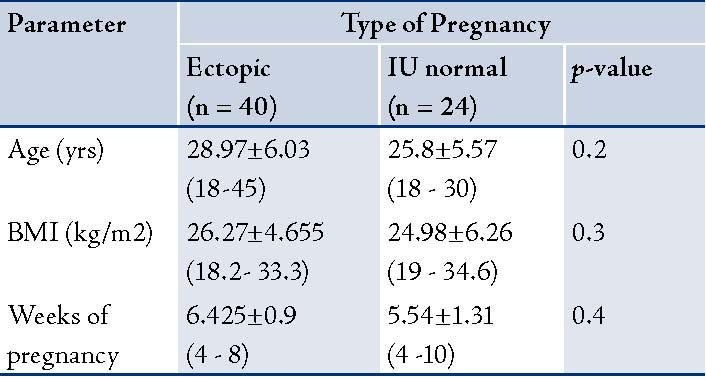 Oman Medical Journal-Archive
Oman Medical Journal-Archive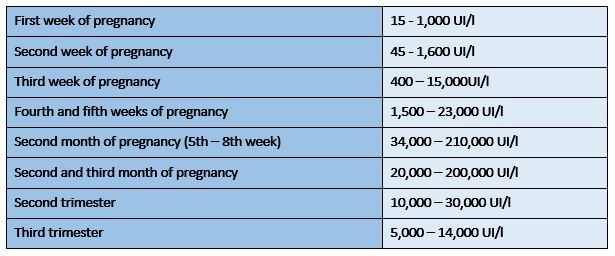 The Two Week Wait (beta hCG) - IVI Fertility clinics
The Two Week Wait (beta hCG) - IVI Fertility clinics beta results chart - Katan.vtngcf.org
beta results chart - Katan.vtngcf.org Biomarkers of Ectopic Pregnancy-Present and Future | IntechOpen
Biomarkers of Ectopic Pregnancy-Present and Future | IntechOpen Signs And Symptoms Of Ectopic Pregnancy At 5 Weeks - Pregnancy ...
Signs And Symptoms Of Ectopic Pregnancy At 5 Weeks - Pregnancy ... Tubal Ectopic Pregnancy - ACOG
Tubal Ectopic Pregnancy - ACOG Ectopic pregnancy - ScienceDirect
Ectopic pregnancy - ScienceDirect Methotrexate treatment in progressive tubal ectopic pregnancies ...
Methotrexate treatment in progressive tubal ectopic pregnancies ... Diagnostic Imaging Pathways
Diagnostic Imaging Pathways![HCG Levels Twins [Definitive Guide]: Chart, 8 Signs, 6 Causes of ... HCG Levels Twins [Definitive Guide]: Chart, 8 Signs, 6 Causes of ...](https://parentslists.com/wp-content/uploads/2019/02/hcg-levels-twins-chart-by-week.jpg) HCG Levels Twins [Definitive Guide]: Chart, 8 Signs, 6 Causes of ...
HCG Levels Twins [Definitive Guide]: Chart, 8 Signs, 6 Causes of ...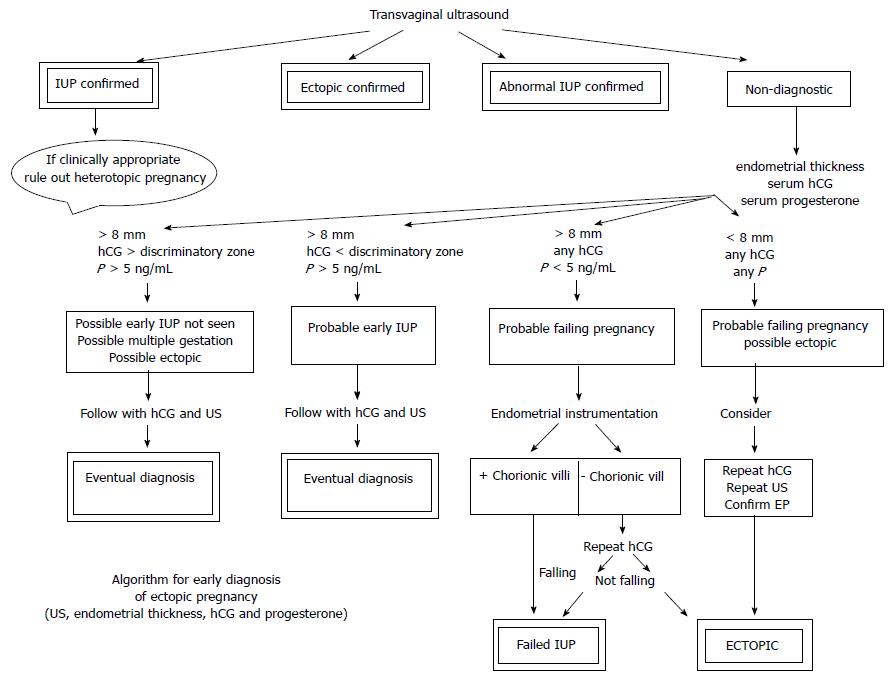 Avoiding misdiagnosing an early intrauterine pregnancy as an ...
Avoiding misdiagnosing an early intrauterine pregnancy as an ...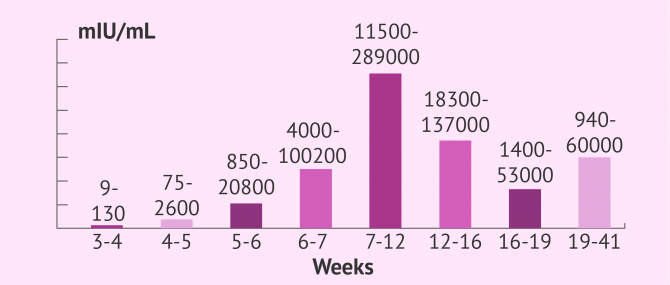 What Are Normal hCG Hormone Levels during Pregnancy?
What Are Normal hCG Hormone Levels during Pregnancy? Calculating Hcg Levels In Pregnancy. IVF beta hCG levels ...
Calculating Hcg Levels In Pregnancy. IVF beta hCG levels ... JPMA - Journal Of Pakistan Medical Association
JPMA - Journal Of Pakistan Medical Association Hcg levels 116 is that to low? - October 2019 Babies | Forums ...
Hcg levels 116 is that to low? - October 2019 Babies | Forums ...
Posting Komentar
Posting Komentar